Dr. M’s Women and Children First Podcast #107: Sundeep Dugar, PhD – Drug Discovery
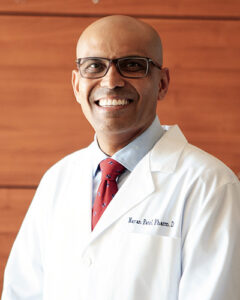
On today’s episode of Dr. M’s Women and Children First Podcast, we welcome a scientist whose work has quietly shaped the cardiovascular health of millions around the world. Dr. Sundeep Dugar is a pharmaceutical innovator, inventor, and industry leader with